The Food and Drug Administration (FDA) quietly allowed a pharmaceutical firm to profit off a life-saving diabetes treatment, shortly after a group of Republican senators proposed legislation to expand access to the treatment by changing how it is regulated.
The FDA on June 28 gave CellTrans Inc., a pharmaceutical company specializing in cellular therapies, approval to sell Lantidra, a pancreatic islet cellular therapy to treat type 1 diabetes. Republican lawmakers led by Utah Sen. Mike Lee had proposed a bill days earlier to recognize islets as organs instead of drugs in order to make islet therapy more accessible.
“Interestingly, the approval came just six days after we presented the bill, and on the same day we informed the FDA about its introduction,” Lee told the Daily Caller in a statement. “While it’s encouraging that this proposed legislation is spurring action, we have serious concerns regarding the drug framework currently used to regulate islets, as there may be more effective approaches for ensuring patient access and safety.”
“Consequently, we are actively engaging with the Department of Health and Human Services and the Food and Drug Administration to obtain further clarification and information on this matter,” he added. (RELATED: EXCLUSIVE: GOP Senators Demand Biden DOJ Provide Answers On CCP Intel-Linked ‘Service Centers’)
4. But here’s one that makes me especially mad: FDA is treating pancreatic islet cells as “drugs” rather than what they are—organs. Consequently, it’s taking forever—just as it does with any “new drug”—to move this new treatment option forward. But it’s not a drug!
— Mike Lee (@BasedMikeLee) April 27, 2023
Most advanced nations recognize islets as organs and tissue for transplantation instead of a drug, according to a July 2020 paper published in the peer-reviewed American Journal of Transplantation.
If islets were regulated as organs, profiting off the treatment would be illegal under the National Organ Transplant Act passed in 1984. Islets are clusters of cells in the pancreas made up of several different kinds of cells, including beta cells that make insulin, according to the University of California San Francisco. Islets are transplanted when they are removed from the pancreas of a deceased organ donor, purified, processed and transferred to a patient.
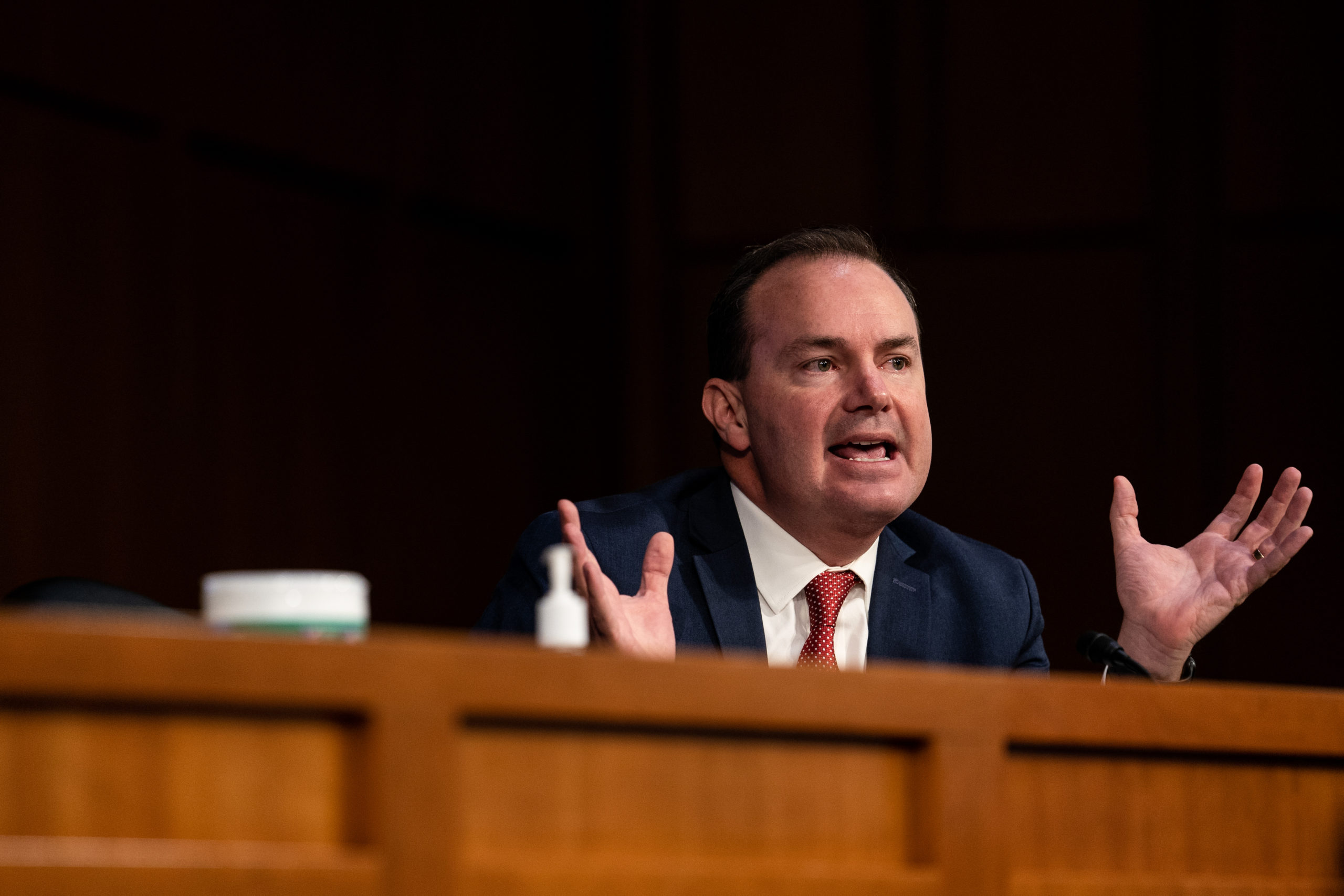
WASHINGTON, DC – OCTOBER 12: U.S. Sen. Mike Lee (R-UT) speaks during Supreme Court Justice nominee Judge Amy Coney Barrett’s Senate Judiciary Committee confirmation hearing for Supreme Court Justice in the Hart Senate Office Building on October 12, 2020 in Washington, DC. (Erin Schaff-Pool/Getty Images)
Republican Senators Lee of Utah, Budd of North Carolina and Blackburn of Tennessee introduced legislation in June to update islet regulation in the Senate and Republican Montana Rep. Matt Rosendale put forward a companion bill in the House.
“This bill holds tremendous potential for those living with this chronic condition, offering the possibility of reducing or eliminating the need for injected insulin,” said Sen. Lee in a press release.
“By redefining islets as organs rather than drugs, we aim to align the regulatory framework with the scientific advancements in the field. This will promote innovation, enhance patient access to islet transplantation, and potentially improve outcomes and quality of life for individuals with Type 1 Diabetes,” Lee added.
Leading scientists in the transplant community endorsed the Republican legislation, including University of Chicago professor and islet transplantation expert Piotr Witkowski. (RELATED: Alzheimer’s Drug Leqembi Gets Full Approval From FDA, Despite Risks)
“The problem is that this will be a single for [profit] company controlling [the] entire field of islet transplantation,” he told the Caller. “The decision can be profit-driven rather than patient best interest driven.”
“This is so disappointing that islet as a drug were approved against advice of the entire transplant community, warning about patient safety compromise, so political and so bad for the patients,” he added.
The American Society of Transplant Surgeons, American Society of Transplantation, Islet for US Collaborative, American Diabetes Association and The Cure Alliance are among the scientific associations supporting the Republican legislation to change how islets are regulated.
14. Currently, the FDA regulates islets as new drugs, which triggers clinical trial and manufacturing requirements. The U.S. is unique in regulating islets as drugs. Many other countries, including Canada, the UK, France, Italy, Australia, and Japan, regulate them as organs.
— Mike Lee (@BasedMikeLee) April 27, 2023
The FDA approved Lantidra for adults with type 1 diabetes who suffer from low blood sugar despite intensive insulin treatment. According to the FDA, Lantidra’s safety was evaluated based on two non-randomized trials involving 30 type 1 diabetes patients and hypoglycemic unawareness, a condition where patients cannot detect when their blood sugar is dropping.
The Lantidra studies cited by the FDA showed 21 patients went a year or more without needing insulin, with 10 participants not needing insulin for more than five years. Five participants did not achieve any days of insulin independence.
Ninety percent of Lantidra users had at least one serious adverse reaction to the drug, according to an FDA package insert with detailed information for patients. The major causes of adverse reactions were the infusion procedure and immunosuppression, the insert states.
CellTrans Inc. will be able to charge patients for the treatment and reap enormous profits because of its seven-year exclusive marketing rights under the Orphan Drug Act. The company did not respond to the Daily Caller’s multiple requests for comment.
Existing FDA regulations have led to a significant decline in the number of patients being treated with islet therapy, according to the Islets for US collaborative, a group made up of dozens of experts. From 1999-2005, 176 type 1 diabetes patients were given islet therapy, compared to 11 between 2016-19, despite the potential for islets to resolve patients’ issues with low blood sugar when insulin therapy is not sufficient.
The FDA’s regulations have also compromised the safety of islet treatment because the FDA’s Biological License Application (BLA) has stalled development in the islet field by preventing clinical usage, Islets for US argued at an April 2021 FDA Advisory Committee meeting in a letter published by the peer-reviewed Journal of Clinical Medicine. CellTrans submitted its BLA request for its islet treatment drug ahead of the FDA meeting.
“The Food and Drug Administration (FDA) has been regulating human islets for allotransplantation as a biologic drug in the US. Consequently, the requirement of a biological license application (BLA) approval before clinical use of islet transplantation as a standard of care procedure has stalled the development of the field for the last 20 years,” the letter reads.
“We provided evidence that BLA requirement and drug related regulations are inadequate in reassuring islet product quality and potency as well as patient safety and clinical outcomes,” the letter continues.
There is no test available to confirm the quality of islets before transplantation and Witkowski believes the drug’s quality puts consumers in harm’s way. (RELATED: FDA Commissioner Calls For Crackdown On Health Misinformation, Claims It Reduces Life Expectancy)
“The worst part is the quality of this drug cannot be reassured. It is not even certain if the drug is sterile and designed to be infused in patient blood circulation. We do not understand how the drug could have [been] approved without confirmation of sterility,” Witkowski said.
“In addition the quality of islets cannot [be] objectively verified and if it doesn’t work we cannot verify that it did not work because the drug is poor quality or there were other reasons,” he added.
Transplant experts at Islets for US made similar arguments about islet safety to the 2021 American Diabetes Association Congress in a report published by the Frontiers in Endocrinology, a peer-reviewed endocrinology journal.
“A recent FDA’s analysis of data submitted by the sponsor to support the BLA, uncovered in our opinion, major deficiencies in current regulations of human islets of deeply concern regarding patient safety and efficacy (4, 5). In contrast to other approved biologics and cell therapies, and despite application of drug manufacturing principles, technology, and regulations, the sterility and potency of islets cannot be verified prior to clinical use,” the report reads.
“This is inconsistent with the principles of the drug safety and efficacy regulatory system developed by the FDA. Yet, the FDA continues to demand that islets be regulated as drugs. This position has halted the development of the field over the last decade in the US, in contrast to other countries worldwide,” the report continues.
The FDA did not respond to the Caller’s request for comment.


